Glaucoma Specialist in Gurgaon
Glaucoma is a typical condition where a group of eye issues damages the optic nerve. The optic nerve is imperative in sending visual information from our eyes to our brain and is very vital for good vision. Thus, this condition can be very harmful to our overall well-being. Damage to the optic nerve is often related to high blood pressure. Glaucoma can happen at any age but is more common in old age people. It is one of the leading causes of blindness for people above the age of 60. So, you should visit a glaucoma specialist soon if you feel any symptoms of the disease.
Dr. Digvijay Singh is the best glaucoma specialist in Gurgaon, India, and is known for bespoke diagnosis and treatment. He has many years of experience in providing glaucoma care and treatment to patients, having treated hundreds of glaucoma cases across India. With his dedication to treating glaucoma, Dr. Digvijay Singh brings his comprehensive knowledge of glaucoma treatment to each individual case he takes on. Amongst various glaucoma specialists in Gurgaon, he is the one who works closely with patients for optimal management and verification tests to ensure that glaucoma can be treated early before any damage occurs. His excellent reputation among both practitioners and patients alike further cements his stature as the best glaucoma specialist in Gurgaon.
He remains devoted to bringing the best glaucoma treatment to his patients. With a deep passion for glaucoma cure and treatment, Dr. Digvijay Singh is the best glaucoma specialist in Gurgaon. Studying it for many years he has vast knowledge and experience in treating glaucoma with success. Patients benefit from his extensive resources as well as cutting-edge technology that helps diagnose glaucoma accurately so they receive the specialized treatments they need. Patients recognize Dr. Singh's commitment to providing superior glaucoma care, making him highly sought after amongst Gurgaon's glaucoma population.
Glaucoma Surgery Specialist Doctor
Dr. Digvijay Singh is an exemplary glaucoma surgery specialist in Gurgaon who brings a wealth of knowledge and experience to his practice. For almost two decades, he has been a prominent glaucoma surgery doctor, providing excellent care for his patients throughout his career. Dr. Singh always puts his patient’s needs first, offering personalized treatment plans that not only tackle glaucoma but also provide long-term results. His passion for glaucoma treatment and knowledge about the condition are unparalleled, making him one of the premier glaucoma surgery specialists in India.
Dr. Digvijay’s commitment to staying up to date on the latest advancements in glaucoma surgery technology ensures that all of his patients can benefit from the most modern treatments available today. With such a level of dedication and expertise, it is no wonder that patients have been trusting him to make life-changing decisions about their glaucoma for years now. He provides specialized glaucoma treatments with the utmost precision and a deep understanding of the eyes and their sensitivities.
Being a renowned glaucoma surgery doctor his continuous ambition and hard work have enabled him to successfully complete multiple glaucoma-related operations with remarkable precision and care. Most patients have expressed great satisfaction with his treatment procedures which often result in lasting improvements to their eyesight or overall health. You can contact him now for all glaucoma-related issues.
Glaucoma can damage your vision so gradually you may not notice any loss of vision until the disease is at an advanced stage. The most common type of glaucoma in the western population is primary open-angle glaucoma, which has no noticeable signs or symptoms. However in India, primary angle closure glaucoma is as frequently seen as primary open angle glaucoma but has is more symptomatic and more blinding.
Early diagnosis and treatment can minimize or prevent optic nerve damage and limit glaucoma-related vision loss. It's important to get your eyes examined regularly, and make sure your eye doctor measures your intraocular pressure.
Types of glaucoma
There are mainly 2 types of glaucoma
1. Open Angle glaucoma/Angle closure glaucoma
2. Narrow angle glaucoma
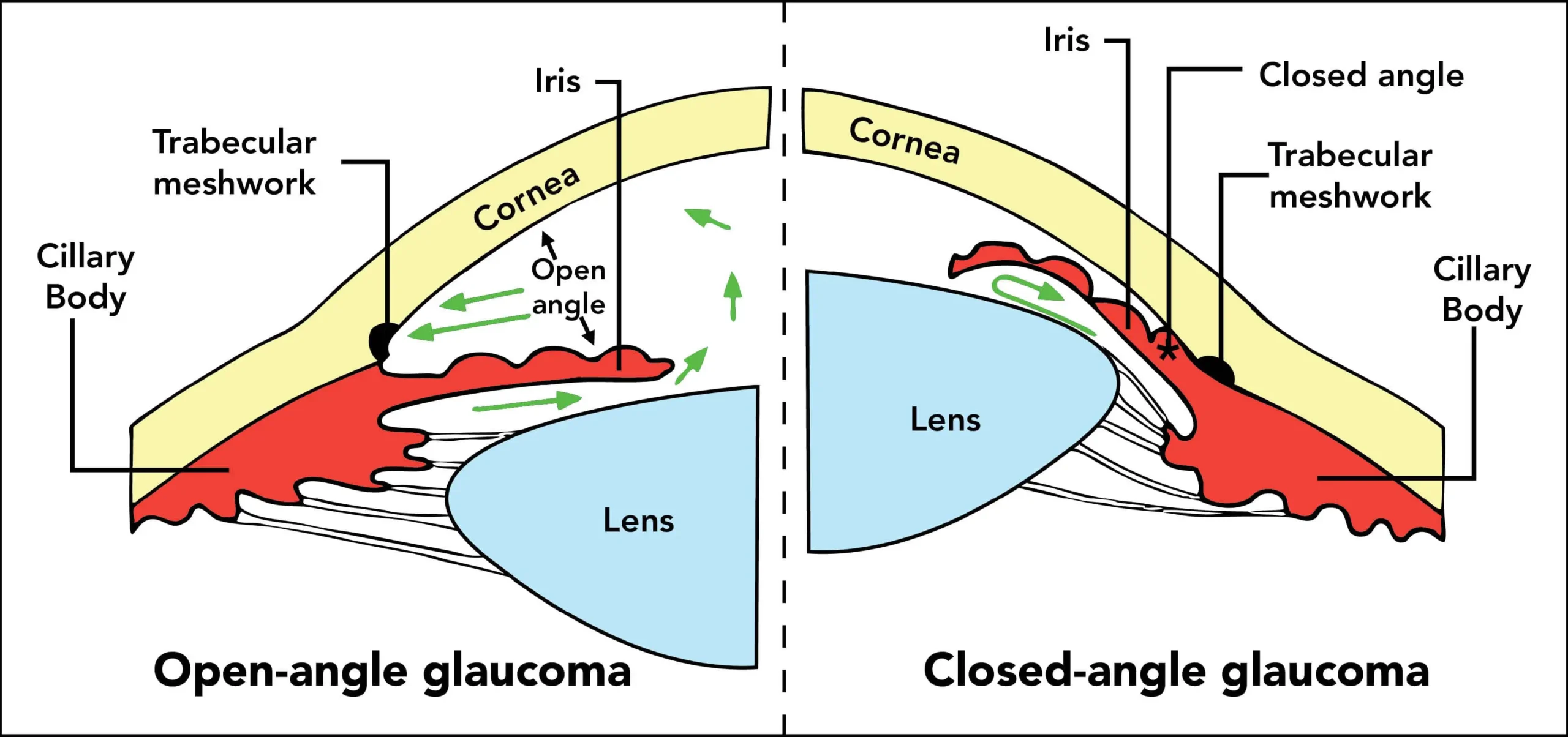
Open angle glaucoma
This is an asymptomatic form of glaucoma which often progresses to advanced stages before detection. However the progression of disease is slower than angle closure glaucoma abd cab be halted with proper medical and laser therapy. In advanced cases, surgery may be needed.
Narrow angle or closed angle glaucoma:
People suffering from this form ofglaucoma would experience pain, redness, and headache which would make you seek the help of an ophthalmologist. Some of these patients would see coloured halos around light bulbs in the evening time though it may also be asymptomatic. It can be treated with laser and may often require surgery.
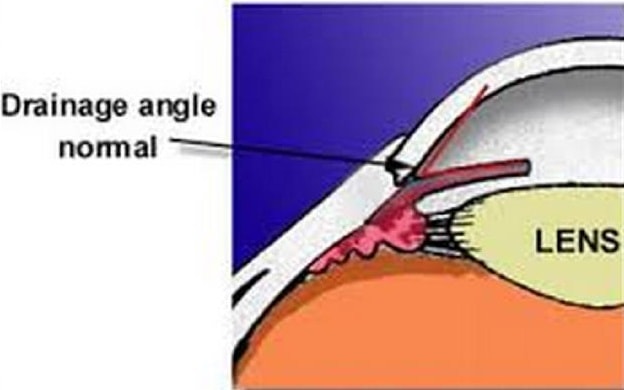
Angle in the Eye
Open versus Narrow/Closed angle
Symptoms of glaucoma
Primary open-angle glaucoma and Narrow angle glaucoma have completely different symptoms.
Primary open-angle glaucoma signs and symptoms include:
· Heaviness, eye pain.
· Gradual loss of peripheral vision, usually in both eyes
· Tunnel vision in the advanced stages
Narrow angle glaucoma signs and symptoms include:
· Eye pain
· Nausea and vomiting (accompanying the severe eye pain)
· Sudden onset of visual disturbance, often in low light
· Blurred vision
· Halos around lights
· Redness of the eye
Both open-angle and narrow angle glaucoma can be primary or secondary conditions. They're called primary when the cause is unknown and secondary when the condition can be traced to a known cause, such as eye injury, medications, certain eye conditions, inflammation, tumor, advanced cataract or diabetes. In secondary glaucoma, the signs and symptoms can include those of the primary condition as well as typical glaucoma symptoms. In a few cases, the glaucoma may be due to both open angle and narrow angle changes in which case it is termed a mixed glaucoma.
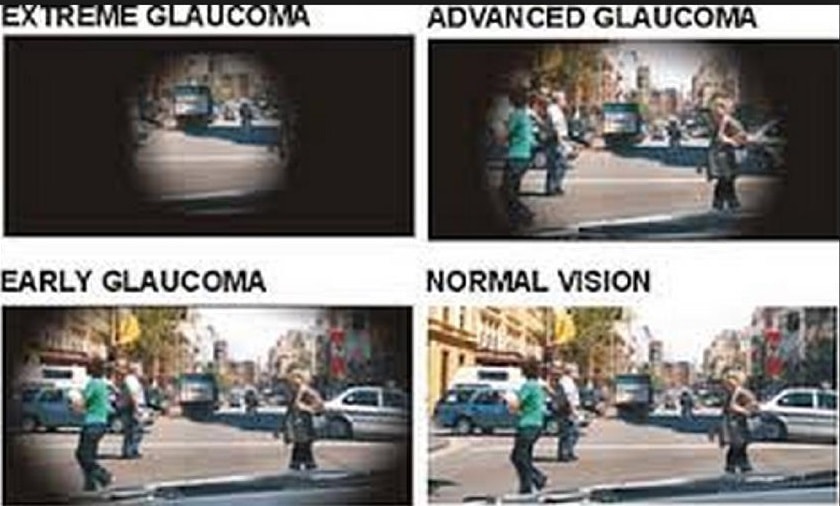
Visual Field Loss in Glaucoma
Causes of glaucoma
For reasons that are not fully understood, increased pressure within the eye (raised intraocular pressure) is usually, but not always, associated with the optic nerve damage that characterizes glaucoma. This pressure is due to a buildup of a fluid (aqueous humor) that flows in and out of the eye.
This fluid normally exits your eye through a drainage system at the angle where the iris and the cornea meet. When the drainage system doesn't work properly, the fluid can't filter out of the eye at its normal rate, and pressure builds within your eye.
· Primary open-angle glaucoma
In primary open-angle glaucoma, the drainage angle formed by the cornea and the iris remains open, but the drainage channels (trabecular meshwork) in the angle are partially blocked, causing the fluid to drain out of the eye too slowly. This causes fluid to back up in your eye, and pressure gradually increases within your eye.
Damage to the optic nerve doesn't cause symptoms or pain, and it happens so slowly that you may lose an extensive amount of vision before you're even aware of a problem. The exact cause of primary open-angle glaucoma remains unknown.
· Narrow angle glaucoma
Narrow angle glaucoma, also called closed-angle glaucoma, occurs when the iris bulges forward to narrow or block the drainage angle formed by the cornea and the iris. As a result, fluid can't adequately flow through and exit your eye, and your eye pressure may increase to very high amounts abruptly. Angle-closure glaucoma usually occurs suddenly (acute angle-closure glaucoma), but it can also occur gradually (chronic angle-closure glaucoma).
Some people with an abnormally narrow drainage angle may be at risk of developing angle-closure glaucoma. If you have a narrow drainage angle, sudden dilation of your pupils may trigger acute angle-closure glaucoma.
· Developmental causes
Some infants or children may be diagnosed with glaucoma. Rarely, some children may be born with glaucoma (congenital glaucoma), develop glaucoma in the first few years of life (infantile glaucoma) or develop glaucoma after age 4 or 5 (juvenile glaucoma). Children with congenital glaucoma may present with irritability, photophobia (intolerance to light), watearing from the eyes and larger looking eyes while patients having juvenile glaucoma usually won't have any symptoms. However, they all will have optic nerve damage, which may be caused by angle blockages or malformations (primary infantile glaucoma), or secondary to other conditions.(secondary glaucoma).
· Other causes
In some glaucoma cases, pigment granules from the iris build up in the drainage channels (trabecular meshwork), slowing or blocking fluid exiting your eye. Physical activities, such as jogging, sometimes stir up the pigment granules, depositing them on the trabecular meshwork and causing intermittent pressure elevations. Over time, the drainage channels may get blocked enough to cause raised eye pressure. Besides pigments, the use of steroids may also lead to a blockage of the drainage system and cause glaucoma (steroid induced glaucoma).
Risk factors of glaucoma
Because chronic forms of glaucoma can destroy vision before any signs or symptoms are apparent, be aware of these factors:
Elevated internal eye pressure (intraocular pressure):
If your internal eye pressure (intraocular pressure) is higher than normal, you're at increased risk of developing glaucoma, though not everyone with elevated intraocular pressure develops the disease.
Age:
You're at a higher risk of glaucoma if you're older. You may be at a higher risk of angle-closure glaucoma if you're older than age 40. For certain groups the risk of developing glaucoma is much higher and occurs at a younger age than that of other groups. If you're 30 years and above you must have regular eye test done.
Family history of glaucoma:
If you have a family history of glaucoma, you have a greater risk of developing it. Glaucoma may have a genetic link, meaning there's a defect in one or more genes that may cause certain individuals to be more susceptible to the disease. A form of juvenile open-angle glaucoma has been clearly linked to genetic abnormalities.
Medical conditions:
Several conditions may increase your risk of developing glaucoma, including diabetes, heart diseases, high blood pressure and hypothyroidism.
Other eye conditions:
Severe eye injuries can cause increased eye pressure. Other eye conditions that could cause increased risk of glaucoma include eye tumors, retinal detachment, eye inflammation and lens dislocation. Certain types of eye surgery also may trigger glaucoma. Smaller sized eyes are at an increased risk of narrow angle glaucoma.
Long-term corticosteroid use:
Using corticosteroid medications, especially eye-drops for a long period of time may increase your risk of developing secondary glaucoma(steroid induced glaucoma).
Test and diagnosis for glaucoma
Your doctor will review your medical history and conduct a comprehensive eye examination. Your doctor may perform several tests to diagnose glaucoma, including:
Visual acuity:
Your doctor will test your ability to see from a distance.
Measuring intraocular pressure by the Applanation Tonometer or the non contact Tonometer:
Tonometry is a simple, painless procedure that measures your internal eye pressure (intraocular pressure), after numbing your eyes with drops. It's usually the initial screening test for glaucoma.
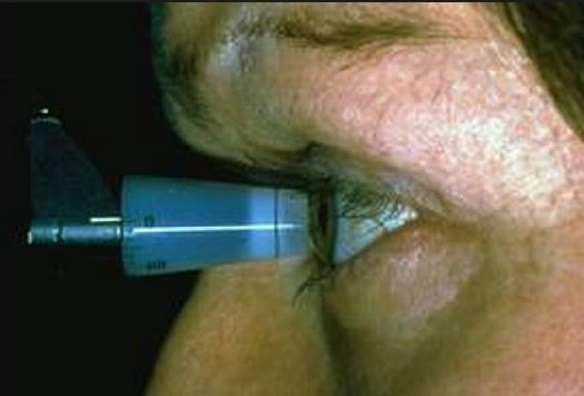
Measuring Intraocular pressure
Test for optic nerve damage:
To check for damage in your optic nerve, your eye doctor uses instruments to look directly through the pupil to the back of your eye(fundus). This can reveal slight changes that may indicate the beginnings of glaucoma.
Gonioscopy:
The doctor will use a special instrument called a gonioscope to view inside your eye to distinguish between open-angle glaucoma and narrow angle glaucoma. The instrument will be gently placed upon the eye after putting some numbing drops for this test.
Visual field test using the Field analyzer:
To check whether your visual field has been affected by glaucoma, your doctor uses a special test to evaluate your peripheral vision.

Visual Fields Machine
Measuring cornea thickness (pachymetry):
Your eyes are numbed for this test, which determines the thickness of each cornea, an important factor in diagnosing glaucoma. If you have thick corneas, your eye-pressure reading may read higher than normal even though you may not have glaucoma. Similarly, people with thin corneas can have normal pressure readings and still have glaucoma.
Special Imaging:
Special imaging tests to evaluate the optic nerve for damage may be done by your eye doctor. These include non-invasive tests like the optical coherence tomography (OCT) and Heidelberg Retinal Tomography (HRT).

Optical Coherence Tomography
Treatments and drugs for glaucoma
The goal of glaucoma treatment is to lower pressure in your eye (intraocular pressure). To treat your condition, doctors may lower your eye pressure, improve drainage of fluid in your eye or lower the amount of fluid produced in your eye.
Eye-drops
Glaucoma treatment often starts with medicated eye-drops. Be sure to use the drops exactly as prescribed, otherwise, your optic nerve damage could get even worse. If your doctor prescribes more than one type of eye-drop, make sure to ask how long to wait between applications and to take the drops for as long as your doctor has prescribed them.
Oral medications
If eye-drops alone don't bring your eye pressure down to the desired level, your doctor may also prescribe oral medications,, to reduce your eye pressure. These medications may cause side effects including nausea, vomiting, gastric upset, frequent urination, a tingling sensation in the fingers and toes, depression, stomach upset, and kidney stones.
Laser
You may have an outpatient procedure called laser trabeculoplasty to treat open-angle glaucoma. After giving you a numbing eye-drop, your doctor uses a high-energy laser beam to open clogged drainage canals and help fluid drain more easily from your eye.
For angle closure glaucoma, a laser procedure called a laser peripheral iridotomy may need to be done by your doctor and it helps increase the angle space and enhance drainage of aqueous humor (fluid)
Your doctor will need to check your eye pressure several times in the following weeks. It may take a few weeks before the full effect of the surgery becomes apparent.
Laser surgery for glaucoma initially lowers pressure in your eye (intraocular pressure). Over time, however, the intraocular pressure may begin to increase and long term medications may be needed.
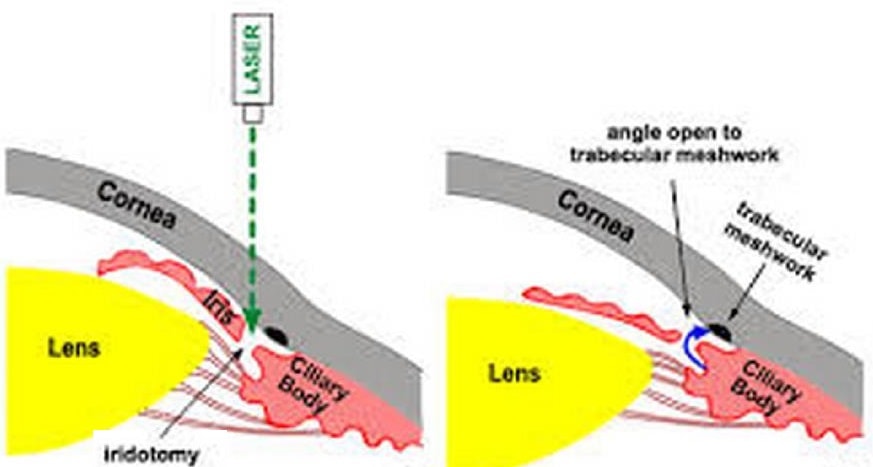
Laser iridotomy for narrow angle glaucoma
Surgery
You may need surgery to treat glaucoma if you can't tolerate medications or if they're ineffective. Sometimes a single surgical procedure may not effectively lower your eye pressure. You may need to continue using eye-drops, or you may need another procedure.
Surgeries that may be performed to treat glaucoma include:
· Filtering surgery:
If eye-drops and laser surgery aren't effective in controlling your eye pressure, you may need a surgical procedure called a trabeculectomy.
This procedure is performed in an outpatient setup. You'll receive a medication to help you relax and usually an injection of anesthetic to numb your eye. Using small instruments under an operating microscope, your surgeon creates an opening in the sclera the white of your eye and removes a small piece of eye tissue at the base of your cornea through which fluid drains from your eye (the trabecular meshwork). The fluid in your eye can now freely leave the eye through this opening. As a result, your eye pressure will be lowered.
Your surgery will be performed on one eye. If necessary, several weeks later you might have surgery on the other eye. You may need additional procedures or treatments, as the opening sometimes heals over or other changes occur in your optic nerve.
Your doctor will check your eye during several follow-up visits, and you'll need to use antibiotic and anti-inflammatory eye-drops to fight infection and scarring of the newly created drainage opening.
Another procedure called trabeculotomy may be performed within the eye which entails removing a targeted strip of the trabecular meshwork with a small tool. Your surgeon inserts the tool into the eye's drainage canal through a small incision at the edge of the cornea and removes the small section of trabecular meshwork. This helps fluid drain more easily from your eye.

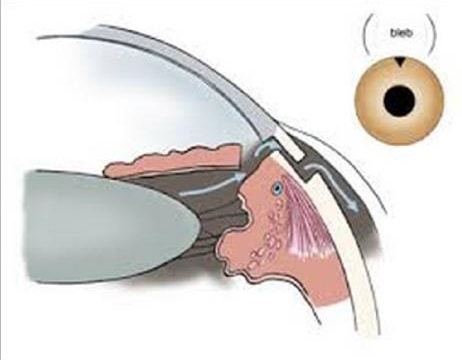
Trabeculectomy surgery for glaucoma
· Drainage implants:
Some people with advanced glaucoma, secondary glaucoma or children with glaucoma may be eligible for drainage implants. Drainage implant surgery takes place in a hospital or an outpatient setup. In this procedure, your eye surgeon inserts a small tube in your eye to facilitate draining fluid (aqueous humor) from your eye to reduce the pressure.
In trabeculectomy and drainage implants, the fluid is directed to a blister (bleb) on the outer layer of your eyeball where it can be absorbed. The bleb will be seen as an elevation in the white portion of the eye though it is mostly hidden under the upper eyelid.
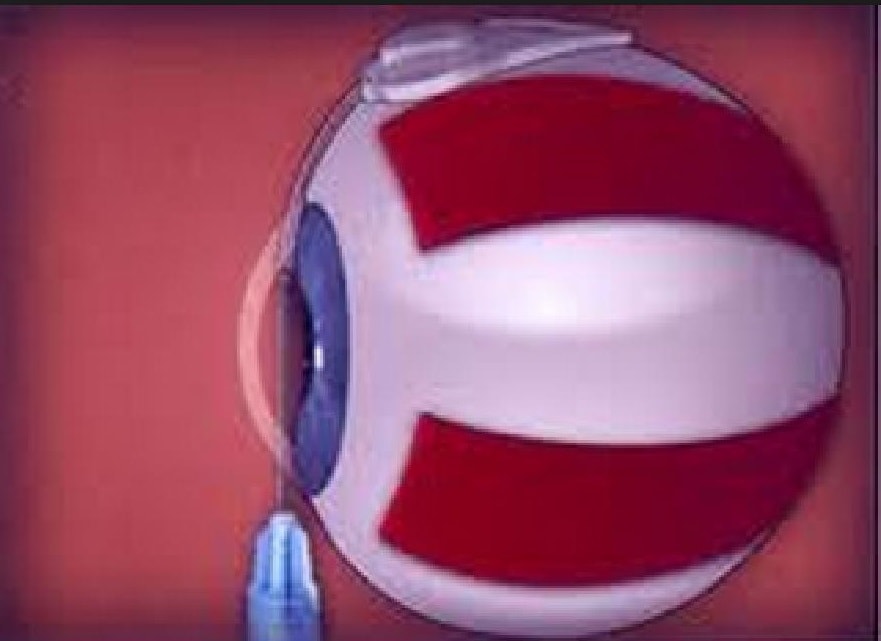
Drainage implant in glaucoma
Prevention of glaucoma
· Get regular eye check up:
Regular comprehensive eye exams can help detect glaucoma in its early stages before irreversible damage occurs. As a general rule, have comprehensive eye exams every three to five years after age 40 and every year after age 60. You may need more frequent screening if you have glaucoma risk factors or are a glaucoma suspect..
· Treat elevated eye pressure:
Glaucoma eye-drops can significantly reduce the risk that elevated eye pressure will progress to glaucoma. To be effective, these drops must be taken regularly even if you have no symptoms.
· Eat a healthy diet:
While eating a healthy diet won't prevent glaucoma, it can improve your physical and mental health. It can also help you maintain a healthy weight and control your blood pressure.
· Wear eye protection:
Serious eye injuries can lead to glaucoma. Keep your eyes protected when you use power tools or play high-speed racket sports on enclosed courts. Also wear hats and sunglasses if you spend time outside.
![DigvijayProfile[1]](https://drdigvijaysingh.com/wp-content/uploads/2017/11/DigvijayProfile1.jpg)
